Understanding Interstitial Cystitis/Painful Bladder Syndrome
Interstitial Cystitis (IC), also known as Painful Bladder Syndrome (PBS), is a chronic pelvic pain condition that affects the bladder, pelvic floor, and surrounding structures. It is far more common in women and often presents with urinary urgency, frequency, bladder pressure, and pelvic pain. While there is no single known cause or cure, effective and evidence-informed treatments exist and pelvic floor physiotherapy is one of the most beneficial.
This blog will help you understand what IC/PBS is, why it happens, and how pelvic floor physiotherapy can significantly improve symptoms and restore quality of life.
⭐ Key Takeaways
IC/PBS causes bladder pressure, urinary urgency and frequency, pelvic pain, and discomfort with intimacy.
The bladder’s communication signals become hypersensitive or dysfunctional.
Pelvic floor dysfunction commonly coexists with IC/PBS and can worsen symptoms.
Pelvic floor physiotherapy helps reduce pain, urgency, frequency, and pelvic muscle tension.
Manual therapy, relaxation strategies, bladder training, and biofeedback are evidence-informed treatment options.
What is Interstitial Cystitis/Painful Bladder Syndrome?
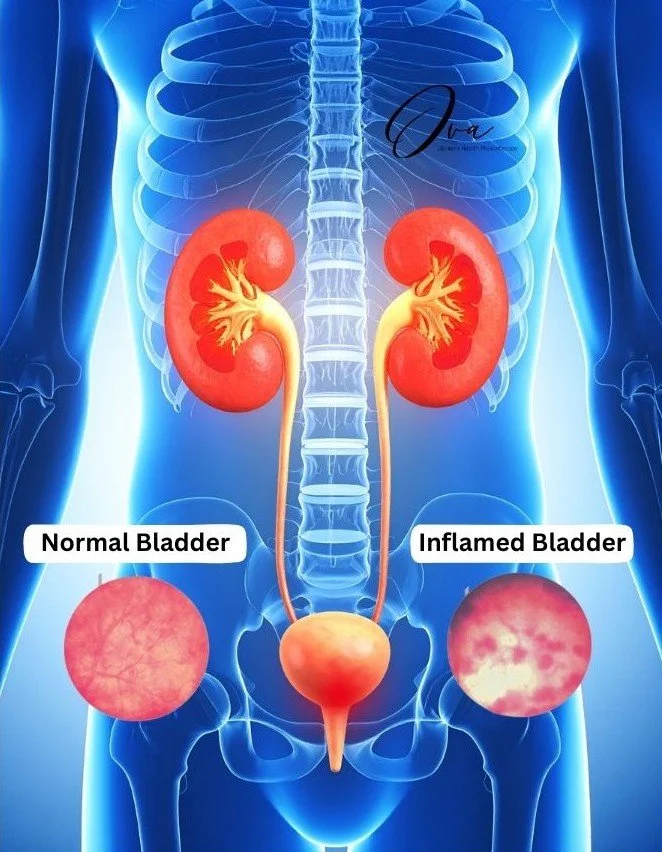
Interstitial Cystitis is a chronic inflammatory bladder condition characterized by sensations of:
Bladder pressure
Pelvic pain
Urinary urgency
Frequent urination with small volumes
The bladder normally expands and signals the brain when it is genuinely full. With IC/PBS, this signalling becomes disrupted. Even a small amount of urine may trigger a strong urge, leading to frequent bathroom visits and significant discomfort.
IC/PBS falls under a group of chronic pelvic pain disorders associated with heightened bladder sensitivity and pelvic muscle dysfunction.
Common Symptoms of IC/PBS
Frequent urination
Many individuals urinate far more than the typical 5 to 8 times daily. This may include waking multiple times during the night.
Urinary urgency
A sudden, strong urge to urinate even when the bladder is not full.
Pelvic or bladder pain
Pain may feel sharp, burning, aching, or pressure-like. Symptoms often worsen with bladder filling and improve after voiding.
Painful intercourse
Pelvic floor tension and bladder irritation can make sexual activity painful.
Small urine volumes
Urination occurs frequently but with small amounts.
What Causes IC/PBS?
The exact cause of IC/PBS remains unknown. Research suggests it likely involves multiple factors, including:
1. Bladder lining defects
A compromised protective lining may allow urine to irritate the bladder wall.
2. Pelvic floor dysfunction
When pelvic floor muscles become tight or overactive, they can compress nerves and contribute to urinary urgency, frequency, and pelvic pain.
3. Autoimmune factors
Some individuals may experience inflammation driven by the immune system.
4. Nervous system hypersensitivity
Changes in pain signalling pathways may make the bladder more sensitive than normal.
5. Previous infections or trauma
Even after an infection clears, the bladder and pelvic floor may remain irritated or sensitive.
Understanding these factors helps guide effective treatment.
How Pelvic Floor Physiotherapy Helps IC/PBS
Pelvic floor physiotherapy is one of the most effective conservative treatments for IC/PBS. Many individuals with IC have overactive, tight, or guarded pelvic floor muscles, which can worsen bladder pain and urgency. Treatment focuses on calming, lengthening, and retraining the deep pelvic support system.
☑️ Pelvic Floor Muscle Rehabilitation
Many IC patients do not need strengthening. Instead, they need:
Improved coordination
Reduced muscle guarding
Decreased internal muscle tension
Better relaxation and lengthening
Correcting these patterns reduces urgency, frequency, and pain.
☑️ Manual Therapy
Pelvic floor physiotherapists use gentle, evidence-informed hands-on techniques to release:
Pelvic floor trigger points
Tight fascia
Bladder-adjacent myofascial restrictions
Abdominal and hip tension
This helps reduce pelvic pain and bladder irritation.
☑️ Relaxation and Down-Training Techniques
IC symptoms often improve when the nervous system becomes calmer. Physiotherapy includes:
Diaphragmatic breathing
Nervous system regulation techniques
Pelvic drop and relaxation exercises
Releasing abdominal and hip tension patterns
These techniques reduce urgency and bladder sensitivity.
☑️ Bladder Training and Behavioural Strategies
Your physiotherapist may guide you with:
Urge suppression strategies
Gradual bladder retraining
Timed voiding
Hydration and fluid timing
Bathroom posture and habits
These lifestyle strategies help stabilize bladder signalling over time.
☑️ Biofeedback
Biofeedback helps individuals:
See real-time pelvic floor muscle activity
Learn how to properly relax the pelvic floor
Reduce overactivity, guarding, and pain
Improve bladder control
Biofeedback is especially effective when pelvic floor tension is contributing to symptoms.
❓FAQs About Interstitial Cystitis/Painful Bladder Syndrome
-
No. IC can feel similar to a UTI, but urine tests do not show an infection.
-
While there is no definitive cure, pelvic floor physiotherapy can significantly reduce symptoms and improve quality of life.
-
Not usually. IC is often linked with pelvic floor overactivity, so relaxation, not strengthening, is the priority.
-
Many individuals notice changes after a few sessions, but long-term improvement often requires consistent treatment over several weeks.
-
Yes. For some individuals, acidic, spicy, or caffeinated foods can worsen symptoms. Your physiotherapist may review bladder-friendly strategies.
Why Choose Ova Women’s Health in Burnaby, BC?
At Ova, we understand how IC/PBS can disrupt every aspect of daily life, from sleep and work to intimacy and emotional well-being. Our care combines advanced pelvic floor rehabilitation with compassionate, specialized support for complex pelvic pain conditions.
✅ Expertise in Complex Pelvic Health
We treat hundreds of women with IC, urgency–frequency syndromes, vulvodynia, and chronic pelvic pain every year.
✅ Evidence-informed pelvic floor physiotherapy
Our focus includes muscle down-training, manual therapy, bladder retraining, and nervous system regulation.
✅ Whole-body, whole-woman approach
We consider pelvic floor dysfunction, posture, stress patterns, diet influences, and bladder behaviour, not just symptoms.
✅ Trusted by women across Burnaby and the Lower Mainland
Patients travel to Ova for our specialized approach to pelvic pain, bladder dysfunction, and complex conditions that require expert care.
Ready to Begin?
Don’t wait. The sooner we start, the sooner you can feel stronger and more supported. Space is limited due to high demand, but if you’re ready to take the first step toward lasting pelvic health, we’re here to help.
📌Related Blogs on Our Website
➡️Painful Intercourse: Why It Happens and How We Treat It
➡️Voiding Difficulties: How Pelvic Floor Physiotherapy Can Help
➡️Vaginismus and the Path to Pain-Free Intimacy
➡️Tight Jaw, Painful Pelvis: The Hidden Link
➡️What’s Causing Your Pelvic Pain?
Want to Learn More? Explore Our Exclusive E-Books, Videos, and Resources
At Ova Women’s Health, we’re not just here to treat; we’re here to educate. If you’re looking for real answers to complex pelvic health concerns, our content goes beyond what you’ll typically find online.
📘 Intimate & Vulvar Hygiene E-Book
A must-read for every woman, especially in early adulthood. This comprehensive guide explains how to care for your intimate area safely and effectively—what to use, what to avoid, and why gentle, evidence-based hygiene is essential for long-term pelvic and sexual health. It’s the foundation of healthy habits that support balance, comfort, and confidence at every stage of life.
📲 Follow us on our Instagram
We share bite-sized, expert-led videos on everything from pelvic pain and sexual health to topics rarely discussed, like vulvar hygiene, oral sex safety, and jaw–pelvic floor connections.
📺 Visit our YouTube channel
For practical guidance and empowering education designed to help you understand your body and feel more in control of your health.
We cover the topics that are often ignored or misunderstood, because women deserve better.